Myocardial segments and coronary artery disease
Introduction
17-Segment Model
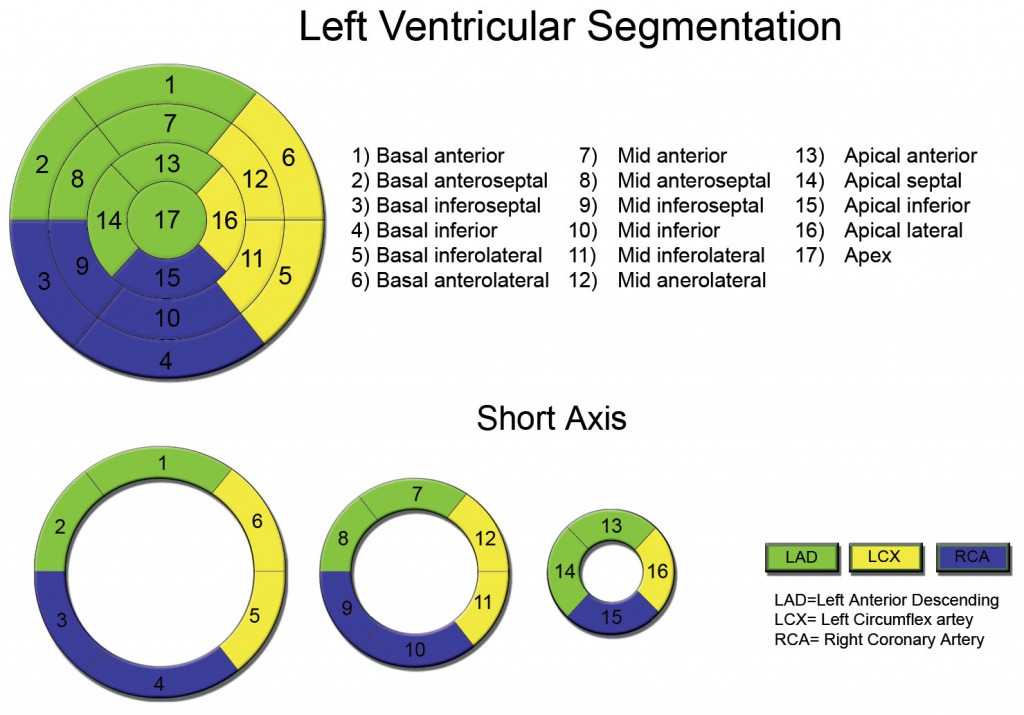
The 17-segment model is a standardised framework used in cardiac imaging to divide the left ventricle (LV) into distinct regions for assessing myocardial function. It groups the LV into three levels—basal, mid-ventricular, and apical—with each level further divided into segments based on their anatomical location: anterior, lateral, inferior, and septal walls. The apex is treated separately as a single segment. This model provides a systematic way to evaluate regional wall motion and correlate abnormalities with the coronary artery territories that supply each segment.
Typically, the left anterior descending artery (LAD) supplies the anterior and septal segments, the left circumflex artery (LCx) supplies the lateral wall, and the right coronary artery (RCA) supplies the inferior wall. Variations in coronary anatomy can lead to overlaps in supply. Clinically, the 17-segment model is crucial for identifying regional wall motion abnormalities (e.g., hypokinesia, akinesia) in coronary artery disease, determining the culprit artery in ischaemia or infarction, and guiding treatment decisions.
This model is often visualised as a bull’s-eye plot, which flattens the LV into concentric rings representing the basal, mid, and apical levels. Strain imaging and speckle tracking echocardiography further enhance its utility by providing segment-specific data on myocardial deformation. By standardising the analysis of LV function, the 17-segment model improves diagnostic precision and communication in clinical practice.
The role of Echocardiography in assessing myocardial segments
Echocardiography is widely used to assess myocardial segments because it provides real-time, detailed imaging of cardiac structure and function, allowing clinicians to identify regional abnormalities with precision. Following a myocardial infarction (MI), certain myocardial segments may exhibit reduced or absent motion, known as hypokinesia or akinesia, as a result of ischaemia or infarction. By using echocardiography, particularly with the 17-segment model, clinicians can systematically evaluate each region of the left ventricle to determine which segments are affected and link these findings to the corresponding coronary artery territory. For example, hypokinesia in the anterior segments of the heart often indicates an occlusion in the left anterior descending artery (LAD).
In addition to visualising wall motion abnormalities, advanced techniques such as strain imaging and speckle tracking echocardiography provide quantitative measurements of myocardial deformation. This allows for early detection of subtle dysfunction, even in cases where ejection fraction remains normal. Furthermore, stress echocardiography can reveal segmental ischaemia that may not be evident at rest, making it invaluable in identifying viable but dysfunctional myocardium for revascularisation planning. The ability to non-invasively detect, localise, and monitor these segmental abnormalities underscores the crucial role of echocardiography in managing conditions like coronary artery disease and post-MI recovery.
Below is a fantastic lecture discussing the use of Echocardiography in detecting regional wall motion abnormalities (RWMAs)
How ischaemia or infarction affects specific segments
Ischaemia or infarction directly affects specific myocardial segments based on the coronary artery territory involved. The heart’s blood supply is divided primarily among the left anterior descending artery (LAD), left circumflex artery (LCx), and right coronary artery (RCA). When one of these arteries becomes occluded, the region of the myocardium it supplies experiences reduced blood flow (ischaemia), leading to impaired contractility. If the occlusion persists, the affected area may undergo infarction (cell death), resulting in permanent dysfunction.
The severity of hypokinesia (reduced movement) or akinesia (absence of movement) depends on the extent of the occlusion and the duration of ischaemia. In the early stages of ischaemia, hypokinesia may be reversible with timely intervention, such as revascularisation through percutaneous coronary intervention (PCI). However, prolonged ischaemia leading to infarction results in scar formation and permanent segmental akinesia or dyskinesia (paradoxical movement).
Echocardiography is critical for assessing this relationship. It allows for the direct visualisation of segmental wall motion abnormalities and their correlation with coronary artery territories. Advanced techniques, such as strain imaging, can detect subtle reductions in myocardial deformation, even before visible hypokinesia occurs, providing crucial insights into the extent and impact of ischaemia or infarction on specific myocardial segments. This information is essential for diagnosing the culprit artery, guiding revascularisation decisions, and assessing prognosis.
Wall motion scoring system
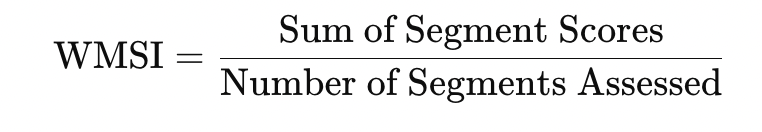
The Wall Motion Scoring System (WMSS) is a method used in echocardiography to systematically evaluate regional myocardial function. It assigns a score to each myocardial segment based on its motion and thickening during systole, enabling a comprehensive assessment of regional and global left ventricular (LV) performance. This system is particularly useful for diagnosing and monitoring coronary artery disease (CAD) and assessing the severity of myocardial dysfunction after ischaemia or infarction.
In the Wall Motion Scoring System (WMSS), myocardial segments are scored from 1 to 4 based on their systolic motion and thickening. A score of 1 indicates normal function, 2 (hypokinetic) reflects reduced motion or thickening (<30%), 3 (akinetic) signifies absent motion, and 4 (dyskinetic) describes paradoxical outward motion. An optional score of 5 may be used for aneurysmal deformation. This system standardises the assessment of regional myocardial function, aiding in the detection of ischaemia or infarction.
Coronary arterty disease quiz – click the segments